- Schedule. Mon - Sat 10.00 - 22.00
RPA in Healthcare
Robotic Process Automation
RPA in Geom Healthcare
At Geom Healthcare, we leverage Robotic Process Automation (RPA) to eliminate repetitive tasks, reduce human error, accelerate cash flow, and deliver 24×7 operational efficiency. Our automation ecosystem is designed specifically for physicians, hospitals, and healthcare systems that demand accuracy, speed, and transparency.
Healthcare Revenue Cycle is filled with routine, rule-based processes that consume time, increase FTE costs, and slow down collections.
- Zero delays
- Zero fatigue
- Zero errors
- Full compliance

Robotic Process Automation
With Geom Healthcare’s RPA, our team will focus on denial management, compliance, and complex tasks—while bots handle the rest.

RPA bots handle front-office workflows with precision.
Tasks Automated
Patient appointment scheduling and rescheduling
Insurance verification during scheduling
Automated reminder messages via SMS/email
Updating patient demographics in EHR
Pre-registration data population
Benefits
Reduced wait times
Error-free demographic entry
Improved patient experience

Automatically identifies denial patterns, payer issues, coding errors, and documentation gaps—helping reduce future denials.
Tasks Automated
Real-time eligibility verification
Benefits extraction (deductible, copay, coinsurance)
Secondary insurance check
Document capture & upload into PMS
Flagging non-covered services
Benefits
Almost zero eligibility denials
70%+ reduction in staff effort
Higher clean-claim rate

Eliminate manual data entry for charges.
Tasks Automated
Pulling charges from EHR
Mapping CPT/ICD codes
Auto-populating modifiers
Updating billing rules
Submitting charges for review
Benefits
Increased coding accuracy
Shorter charge-to-bill cycle
Higher claim acceptance
Automate both ERA and non-ERA payments effortlessly.
Tasks Automated
ERA auto-posting
Manual EOB interpretation
Splitting payments by line item
Adjustments & write-offs
Posting secondary balances
Benefits
100% accuracy
Faster reconciliation
Reduced posting backlog
Bots categorize and route denials instantly.
Tasks Automated
Auto-reading payer responses
Categorizing by denial type
Assigning to respective teams
Filing corrected claims
Tracking resolution progress
Benefits
40–60% reduction in denial turnaround
No missed or untouched denials
Higher recovery rate
Bots follow up with payers so staff can focus on complex cases.
Tasks Automated
Working AR aging buckets
Checking claim status on portals
Identifying next action
Auto-creating follow-up notes
Triggering tasks for staff when escalation is needed
Benefits
Faster AR cleanup
Reduced DNFB
Increased cash flow
Bots improve communication and reduce billing queries.
Tasks Automated
Auto-generating patient statements
Sending reminders for unpaid balances
Payment link sharing
Logging communication history
Benefits
Better patient collection rates
Reduced outbound calls
Improved financial clarity for patients

RPA bots handle front-office workflows with precision.
Tasks Automated
Patient appointment scheduling and rescheduling
Insurance verification during scheduling
Automated reminder messages via SMS/email
Updating patient demographics in EHR
Pre-registration data population
Benefits
Reduced wait times
Error-free demographic entry
Improved patient experience

Automatically identifies denial patterns, payer issues, coding errors, and documentation gaps—helping reduce future denials.
Tasks Automated
Real-time eligibility verification
Benefits extraction (deductible, copay, coinsurance)
Secondary insurance check
Document capture & upload into PMS
Flagging non-covered services
Benefits
Almost zero eligibility denials
70%+ reduction in staff effort
Higher clean-claim rate

Eliminate manual data entry for charges.
Tasks Automated
Pulling charges from EHR
Mapping CPT/ICD codes
Auto-populating modifiers
Updating billing rules
Submitting charges for review
Benefits
Increased coding accuracy
Shorter charge-to-bill cycle
Higher claim acceptance
Automate both ERA and non-ERA payments effortlessly.
Tasks Automated
ERA auto-posting
Manual EOB interpretation
Splitting payments by line item
Adjustments & write-offs
Posting secondary balances
Benefits
100% accuracy
Faster reconciliation
Reduced posting backlog
Bots categorize and route denials instantly.
Tasks Automated
Auto-reading payer responses
Categorizing by denial type
Assigning to respective teams
Filing corrected claims
Tracking resolution progress
Benefits
40–60% reduction in denial turnaround
No missed or untouched denials
Higher recovery rate
Bots follow up with payers so staff can focus on complex cases.
Tasks Automated
Working AR aging buckets
Checking claim status on portals
Identifying next action
Auto-creating follow-up notes
Triggering tasks for staff when escalation is needed
Benefits
Faster AR cleanup
Reduced DNFB
Increased cash flow
Bots improve communication and reduce billing queries.
Tasks Automated
Auto-generating patient statements
Sending reminders for unpaid balances
Payment link sharing
Logging communication history
Benefits
Better patient collection rates
Reduced outbound calls
Improved financial clarity for patients
Solution that inspire Progress
At Geom Healthcare, expertise isn’t just a capability—it’s the foundation of everything we deliver. Our team brings decades of experience across physician practices, hospitals, specialty groups. With deep knowledge of payer rules, compliance guidelines, coding standards, and RCM workflows, we ensure that every process we handle is executed with precision.
Our performance is defined by measurable, predictable results that directly impact your bottom line. Every workflow we design aims at speed, clarity, efficiency, and maximum reimbursement. With automation and analytics at the core, we consistently exceed industry benchmarks.
Quality is embedded in every step of your revenue cycle with Geom Healthcare. Through continuous monitoring, RPA-driven accuracy, and standardized workflows across all specialties, our team ensures world-class billing performance with minimal errors.
At Geom Healthcare, expertise isn’t just a capability—it’s the foundation of everything we deliver. Our team brings decades of experience across physician practices, hospitals, specialty groups. With deep knowledge of payer rules, compliance guidelines, coding standards, and RCM workflows, we ensure that every process we handle is executed with precision.
Our performance is defined by measurable, predictable results that directly impact your bottom line. Every workflow we design aims at speed, clarity, efficiency, and maximum reimbursement. With automation and analytics at the core, we consistently exceed industry benchmarks.
Quality is embedded in every step of your revenue cycle with Geom Healthcare. Through continuous monitoring, RPA-driven accuracy, and standardized workflows across all specialties, our team ensures world-class billing performance with minimal errors.
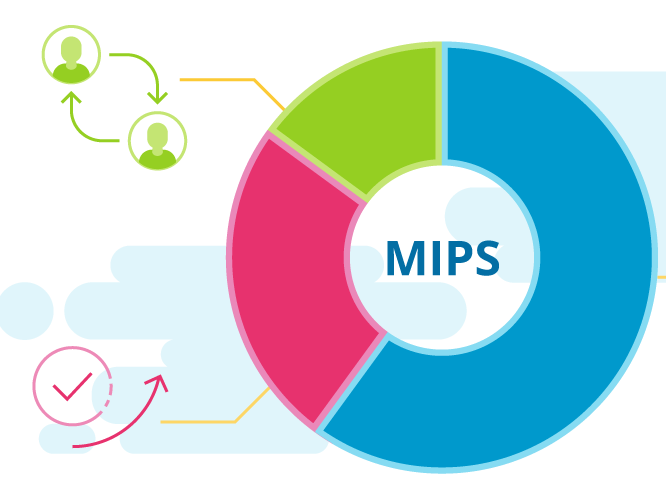
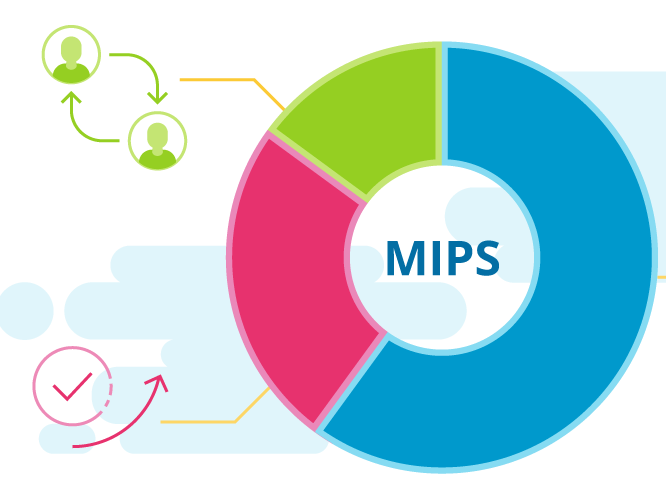
Why Choose Us Over Others
| Feature / Benefit | Geom Healthcare | Other RCM Companies | In-House Billing |
|---|---|---|---|
| 24×7 Operations | ✓ Yes | ✘ Mostly No | ✘ No |
| 24-Hour Billing TAT | ✓ Guaranteed | ✘ Not Guaranteed | ✘ Usually 48–72 hrs |
| Free KPI Dashboards | ✓ Included | ✘ Extra cost | ✘ Must purchase |
| AI & RPA Automation | ✓ Strong automation | ✘ Limited | ✘ Rarely used |
| Predictive Denial Analytics | ✓ Yes | ✘ Minimal | ✘ None |
| Scalability | High | Medium | Low |
| Staff Stability | Guaranteed | Varies | High turnover risk |
| Specialty Expertise | 20+ specialties | Limited | Depends on staff |
| Cost Efficiency | High | Medium | Low |
| Reporting Transparency | Real-time dashboards | Basic monthly reports | Limited |
Top 4 Steps for New Project or Practice Implementation
Initial Assessment & Requirements Gathering
Credentialing, Contracting & System Setup
Workflow Design & Staff Training
Go-Live Support & Performance Monitoring
Have any Question?
Have any questions? Our team is here to help you with RCM, billing, credentialing, or any service you need. Just fill out the form and we’ll get back to you shortly.
